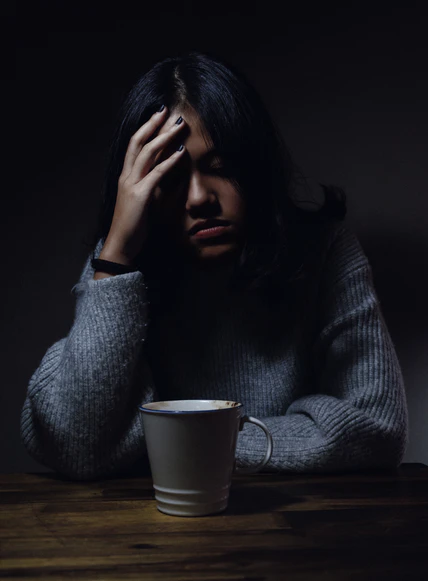
Photo by Anh Nguyen on Unsplash
You feel as if you’ve just finished a marathon and added to that you have what seems like the worst jetlag ever… it’s like trudging through mud, muscles aching, head so foggy you wish you could blow the cobwebs out and think straight for a change. Even taking a deep breath is difficult and sometimes you just can’t get enough air.
This is the reality for many people with Long-Covid.
Previously fit and healthy people, who led productive lives before a bout of COVID-19, suddenly find themselves struggling to cope with everyday life, sometimes severely debilitated and unable to work, study or take part in everyday activities. Fatigue, breathlessness, brain fog, sleep issues, and cough are just a few of the symptoms associated with Long-Covid.
In this blog post I will address some of the issues surrounding Long-Covid, in particular a possible link with breathing, which may be associated with one subgroup of people experiencing Long-Covid.
The medical name for Long-Covid is: “Post-Acute Sequelae of SARS-CoV-2 Infection” or “Long-Covid Syndrome”. Currently there are several theories as to why people develop Long-Covid, a condition generally defined as being present when symptoms persist for longer than three months following COVID-19 infection.
Research is ongoing but finding a cause for Long-Covid has scientists baffled. It may require a huge amount of scientific detective work to find a cause, but hopefully some treatments or even a cure may be found.
There are few clues as to what underlies Long-Covid. It appears to strike indiscriminately. Males and females, adults and children, young and old, vaccinated and unvaccinated, with a history of mild to severe COVID-19 infection may be affected. There are some variations in the percentages impacted within these groups, e.g., reports indicate that females are affected in greater numbers than males, as are more unvaccinated than vaccinated people.
To date, areas of research on Long-Covid include:
- Similarities with other post-viral conditions such as glandular fever (Epstein-Barr).
- Similarities with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS).
- An immune system response. Immune system biomarkers (proteins) found in the blood of patients with Long-Covid have been detected by Australian researchers. These proteins generally disappear following an acute infection but in Long-Covid patients they were found to be present for extended periods, suggesting the immune system may remain “switched on”. If successful, this study could pave the way for treatments.
- Abnormal breathing patterns.
Abnormal breathing patterns and Long-Covid
Preliminary research suggests that there may be an association between Long-Covid and abnormal breathing patterns in one subset of Long-Covid patients. These studies generally relate to patients referred by specialists who had found no evidence of underlying organ damage or inflammation following COVID-19 infection.
An American College of Cardiology press release from 2021 describes research on breathing with Long-Covid patients which found that 88 per cent of patients studied exhibited abnormal breathing patterns. Low carbon dioxide values at rest and with exercise were found in this study. Researchers say that these findings are suggestive of chronic hyperventilation, which may underlie symptoms. Further, almost half of the patients in this study were found to meet the criteria for ME/CFS.
A study in Sweden during 2020-2021 researched breathing patterns in patients with Long-Covid during exercise and found that a third of patients had an abnormal breathing pattern combined with reduced exercise capacity.
Similar to the USA study mentioned, findings from a 2021 UK study found that 87 per cent of participants showed disordered breathing on initial testing. Findings also suggest that 69 per cent had hyperventilation syndrome (a chronic form of hyperventilation). Researchers concluded that a six-week course of breathing retraining combined with energy management was found to be beneficial for Long-Covid patients.
Improvements were found in several of the areas studied, including breathlessness and fatigue – two of the main symptoms of Long-Covid. In addition, over half of the participants had a clinically significant improvement in anxiety and depression.
Researchers from this pilot study say that further research is required to determine the effectiveness of breathing retraining and energy management plans for this subset of Long-Covid patients.
Breathing and stress
For 20 years prior to the pandemic, I taught breathing retraining to clients experiencing stress, anxiety and panic.
When we are stressed, our breathing, heart rates and blood pressures increase due to sympathetic nervous system arousal (we know this as the fight-or-flight response). Following a period of prolonged or extreme stress, hyperventilation may become a habit in some people.
Some clients described a history of illness, surgery, or trauma which, they said had precipitated their symptoms. Others recounted a history of psychological or emotional issues which had affected their health. Many reported symptoms such as fatigue, brain fog, poor or unrefreshing sleep, exercise intolerance, muscle pain, shortness of breath and loss of confidence.
To assess and monitor my clients’ breathing I used a non-invasive instrument called a “capnometer”. This instrument displayed their breathing pattern in wave form on a screen, so they could clearly see what was happening. In addition, their breathing and heart rates were displayed. But the most significant measurement assessed with this instrument was the end-tidal carbon dioxide values, mentioned earlier.
Carbon dioxide levels in the majority of clients were low, suggesting hyperventilation. Hyperventilation is not a modern-day phenomenon; it has been with us for centuries. Stress is usually the precursor to hyperventilation which may then lead to numerous symptoms.
The pandemic has been an extremely stressful time for most people but for people who develop COVID-19 this adds extra layers of stress, including physical illness and the stress of not knowing how severe their illness will be or the outcomes.
Could stress be the link to at least some of the current incidence of Long-Covid and the possible aftermath of abnormal breathing patterns including hyperventilation?
Hyperventilation: what happens?
Hyperventilation leads to a disturbance in the balance of gases (carbon dioxide and oxygen) in the body. Excessive amounts of carbon dioxide are exhaled, putting a strain on the body and leading to symptoms. Carbon dioxide is not just a waste gas. Levels within a very specific range are necessary for several body processes, including the effective release of oxygen from our red blood cells.
The breathing pattern in hyperventilation may be shallow and rapid, but this is not always the case. In my experience, some people may have a normal respiration rate but when assessed on capnometry their carbon dioxide values are found to be low, suggesting hyperventilation.
Sometimes we assume that hyperventilation involves loud, noisy or noticeably deep breathing. Generally, this is not the case; hyperventilation is usually quiet and may not be obvious.
People who are hyperventilating are sometimes not aware that they are over-breathing, in my experience. They are more likely to describe difficulty in breathing, a “hunger for air” or a sensation that no matter how deeply they breathe they can never get enough air. They may describe shallow breathing, tightness in the chest, or periods when they “stop breathing” for a while and then resume with a bigger breath. Excessive sighing and yawning may also be present. Just talking on the telephone may trigger shortness of breath in some people. Exercise can also be difficult (assuming they are not too fatigued to exercise) as they may find it difficult to breathe while exercising.
Shortness of breath, fatigue, poor sleep, brain fog, and muscle aches and pains may be found in association with hyperventilation. People experiencing Long-Covid may relate to these symptoms; they are virtually identical to the Long-Covid list of symptoms quoted in media reports and research papers.
Conclusions
According to research reports, Long-Covid in a subset of patients may be associated with abnormal breathing patterns, a finding which researchers say is important as breathing issues may be addressed with breathing exercises or breathing retraining.
However, current research on this topic is limited and further research is needed. Hopefully this can be carried out in the near future.
I am now retired, but when I taught breathing retraining I saw first-hand how disordered breathing can impact people’s lives, in particular their health, wellbeing and confidence levels. I also witnessed how effective breathing retraining can be in alleviating symptoms and restoring health.
Mary Birch is the author of Breathe The 4-week breathing retraining plan to relieve stress, anxiety and panic, 2019, Hachette Australia, and Piatkus, UK.
Information provided in this blog post is general in nature and is not intended as a substitute for medical advice and must not be relied upon as such. For all healthcare advice, always consult a healthcare practitioner.
© Mary Birch 2022